Depression
What is Depression?
Depression is more than just feeling sad or having a bad week. It’s a real medical condition that affects how you think, feel, and function. Also known as Major Depressive Disorder, depression is characterized by a persistently low mood or loss of interest in activities you once enjoyed, lasting for weeks or longer. It can happen to anyone, from university students overwhelmed by life changes, new immigrants adjusting to a new normal without their support systems, to new parents dealing with postpartum depression. Depression doesn’t mean you’re “weak” or failing; it’s a common mental health condition that millions face and the right treatment can help.
Symptoms of Depression
Depression can look different for everyone, but common symptoms include:
Persistent low mood or sadness: Feeling empty, hopeless, or tearful most days.
Loss of interest or pleasure: Activities and hobbies you once enjoyed may no longer appeal to you.
Changes in appetite or weight: Significant weight loss or gain, or noticeable changes in eating habits.
Sleep disturbances: Insomnia (difficulty sleeping) or oversleeping nearly every day.
Fatigue and low energy: Feeling exhausted, drained, or “slowed down” almost all the time.
Feelings of guilt or worthlessness: Excessive self-blame or feeling like you’re “not good enough.”
Difficulty concentrating: Trouble focusing, making decisions, or remembering things.
Thoughts of death or suicide: In severe cases, recurring thoughts of not wanting to live (if you experience these, seek emergency help immediately).
It’s important to note that a person with depression might not have all these symptoms. Generally, if you’ve been experiencing several of these signs most days for two weeks or more, it may be a sign of clinical depression rather than a passing “down” mood. You are not alone, and support is available.
World Health Organization. “Depressive disorder (depression)” — Fact sheet.
How Psychotherapy Helps with Depression
Depression is treatable, and psychotherapy (“talk therapy”) is a proven path to healing. Addy Psychotherapy takes an evidence-based approach, drawing on therapies like Cognitive Behavioral Therapy (CBT), Acceptance and Commitment Therapy (ACT), and Dialectical Behavior Therapy (DBT), among others. Here’s how therapy can help:
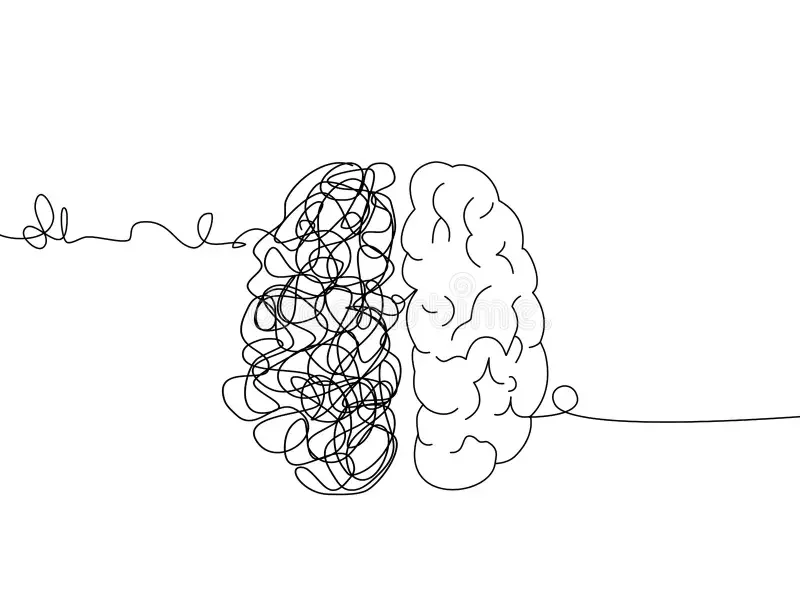
Identify and change negative patterns: In depression, our minds often get stuck in loops of negative thoughts (“I’m worthless,” “Nothing will ever get better”). CBT helps you recognize these unhelpful thoughts and challenge them, gradually replacing them with more balanced, realistic thinking. This isn’t “positive thinking” fluff; it’s a skill that research shows can significantly improve mood and functioning.
Reconnect with activities and hope: Depression can make you withdraw from life. Techniques like behavioral activation, will help you engage in meaningful activities again, even in small steps. Regaining a sense of routine or doing things that once mattered to you (like taking a walk, calling a friend, or a creative hobby) can start to lift the fog.
Process pain and build coping skills: For some, depression stems from difficult life events such as grief, trauma, or major life transitions. Therapy provides a safe, non-judgmental space to work through these feelings. Approaches like ACT help you accept painful emotions and commit to actions aligned with your values (for example, valuing family enough to seek help to be present for them). Meanwhile, DBT can teach practical skills for managing overwhelming emotions and finding moments of positivity even during dark times.
Support and perspective: Importantly, therapy offers a caring, confidential relationship where you are truly heard. Simply talking to a trained professional can bring relief and new perspective. Many clients say that having a therapist who “gets it” and validates that depression is real – while also gently challenging them to take small steps forward – makes a huge difference in recovery. You’ll learn that you don’t have to battle depression alone.
Sometimes therapy is used on its own, and other times it’s combined with medication – it depends on the individual. Research shows that a combination of therapy and antidepressant medication can be very effective for moderate to severe depression, often more than either approach alone . Our therapists can work closely with your family doctor or psychiatrist if you are considering medication, ensuring you get well-rounded care. Whether or not you take medication, psychotherapy is a key part of overcoming depression, because it equips you with lifelong skills and strategies to maintain your mental health.
Common Misconceptions About Depression and Therapy
-
Depression is a legitimate medical illness, not a character flaw. You wouldn’t call someone with diabetes “weak” for having low insulin; similarly, having depression isn’t your fault. It results from a complex mix of biological, psychological, and situational factors. Seeking help for depression means you’re strong enough to recognize you deserve support.
-
You can’t simply will away depression by “thinking positively” or “trying harder.” Just like a broken leg needs treatment, a depressed brain often needs professional support. Many people try to tough it out alone, but depression can be persistent and may worsen if untreated . Therapy and/or other treatments provide tools to truly heal, not just suppress symptoms.
-
Therapy is not just venting; it’s working actively with a professional who can guide you to solutions. Evidence-based therapies for depression have decades of research behind them showing they do create real improvements in the brain and mood. Therapists use structured techniques (like CBT) to help you change negative thought patterns and behaviors. Over time, most people feel the difference – they start enjoying life again, solving problems effectively, and thinking more clearly. In short, therapy addresses root causes and provides concrete skills, not just talk.
-
You are in control of your therapy. While getting to the heart of certain issues can be helpful, you won’t be forced to discuss traumas or secrets before you feel safe. Therapists are trained to proceed at your pace. It’s okay to let your therapist know if something is too hard to talk about yet. They can work with you to build coping skills first or approach tough topics gradually. Your comfort is a priority – healing is not a forced march, but a guided journey.
-
Medication can be very useful for some people, but it’s not the only answer. Depression does often involve brain chemistry – but therapy can actually lead to positive chemical and structural changes in the brain as well. For mild to moderate depression, therapy alone is often enough to achieve recovery. For more severe depression, many find the best results with a combination of therapy and medication . Regardless, therapy is crucial because it teaches you strategies to cope and prevent future depressive episodes. Antidepressants can adjust brain chemistry, but therapy empowers you to change the thoughts and habits that fuel depression.
FAQs
How do I know if I’m really depressed or just going through a rough patch?
It’s normal to feel down or stressed from time to time, but depression tends to be more intense and long-lasting than everyday sadness. Key signs of depression include a low mood or loss of interest in things you usually enjoy, along with other symptoms (like changes in sleep, appetite, energy, or self-worth) that persist for two weeks or more . Think about how these feelings affect your daily life: if it’s getting hard to function at work or school, or to maintain relationships, that’s a red flag. “Normal” sadness usually lifts on its own with time, but depression can linger or worsen if untreated. If you suspect you might be depressed, consider reaching out for a professional assessment – you don’t have to wait until things become very severe. Early support can prevent a deeper decline. Remember, whether it’s “clinical depression” or not, if you’re suffering, you deserve help and understanding.
Do I need medication for my depression, or can therapy alone help?
This depends on the severity of your depression and personal preferences. Many individuals with mild to moderate depression improve greatly with psychotherapy alone. Therapies like CBT have been shown to work as well as medications for many people, by teaching skills to manage depressive thoughts and behaviors. For more moderate to severe depression, medication can sometimes be important in addition to therapy – antidepressants can lift your mood enough to engage more effectively in therapy. Research indicates that combining medication with therapy can be the most effective approach for harder-to-treat depression . That said, medication is not a “must” for everyone. Our approach is to start where you’re comfortable: if you prefer to try therapy first without meds, that’s completely fine. We can monitor your progress together. If symptoms are very intense (for example, if you’re barely able to get out of bed or having frequent suicidal thoughts), we might discuss consulting a doctor about possibly adding medication for extra support. Any medication decisions would be made collaboratively – your informed choice is key. Remember, therapy itself is a powerful treatment: it helps fix the underlying patterns contributing to depression, whereas medication alone doesn’t teach you coping skills. Many people either don’t need meds or use them short-term while gaining long-term tools from therapy. We’ll work with you and any other healthcare providers to find the best plan for you.
This is a frequently asked question?
It all begins with an idea. Maybe you want to launch a business. Maybe you want to turn a hobby into something more. Or maybe you have a creative project to share with the world. Whatever it is, the way you tell your story online can make all the difference.
What can I expect from therapy for depression?
Depression therapy is typically a weekly (or biweekly) conversation with a trained mental health professional in a safe, confidential setting (in-person or online). In the first session(s), your therapist will get to know you – asking questions about what you’re going through, your background, and your goals for therapy. This helps them tailor a treatment plan for you. As sessions progress, you might work on: identifying negative thought patterns, learning coping techniques (for example, how to ground yourself during a wave of sadness or anxiety), and setting small achievable goals (like establishing a routine or re-engaging in a hobby). Therapists often give homework – perhaps a journal exercise or practicing a skill between sessions – so you continue healing in daily life. Over time, therapy becomes a collaborative process: you’ll share what’s working or not, and your therapist will adjust strategies accordingly. Many people start noticing small improvements in mood or motivation after a few sessions, and significant improvement can often be seen after about 10–15 sessions (a few months) , though everyone’s timeline is different. Above all, you can expect therapy to be supportive and non-judgmental – it’s a space for you to be heard and to learn ways to feel better.
What if I can’t pinpoint why I’m depressed? Can therapy still help?his is a frequently asked question?
Yes, absolutely. It’s not uncommon to feel depressed without knowing exactly why. Depression can arise due to a mix of factors – some internal (like genetics or brain chemistry) and some external (like stress or loss) – and sometimes it seemingly “just happens.” You don’t need to have a obvious reason (such as a trauma or major loss) for your feelings to be valid. Therapists are skilled at helping you explore and make sense of your experience, but even if a clear cause isn’t found, therapy will focus on improving your mood and functioning in the here and now. We might work on establishing healthier daily routines, challenging any harsh self-critical thoughts you didn’t realize you had, or finding small sparks of joy and meaning to gradually brighten your outlook. Imagine depression as a fog – you may not know what caused the fog, but therapy can teach you how to navigate through it and eventually clear the skies. Many clients say that over the course of therapy, they come to understand personal triggers or patterns contributing to their depression (for example, people-pleasing leading to burnout, or suppressed emotions from years past). But even if the origin remains a mystery, what matters is that you start feeling better. In short, knowing “why” is less important than knowing “what now” – and therapy is very much about the what now. It gives you strategies to cope and climb out of depression regardless of how you fell in.
This is a frequently asked question?
It all begins with an idea. Maybe you want to launch a business. Maybe you want to turn a hobby into something more. Or maybe you have a creative project to share with the world. Whatever it is, the way you tell your story online can make all the difference.
Therapy for Depression
How can therapy help with depression?
Therapy provides a structured and supportive space to understand the root causes of depression and learn strategies to manage it. Evidence-based approaches such as cognitive behavioural therapy (CBT), interpersonal therapy, and trauma-informed care have been shown to reduce symptoms, improve mood, and restore daily functioning.
How long does it take to feel better with therapy?
The timeline varies. Some people notice changes after a few sessions, while others may require several months of steady work. What matters is consistency and the fit between you and your therapist.
Can therapy help with both depression and other issues like anxiety or trauma?
Absolutely. Depression often overlaps with anxiety, trauma, or relationship difficulties. Therapy addresses these interconnected challenges, giving you tools to manage them together rather than in isolation.
Is therapy effective if I’ve been depressed for years?
Yes. Even when depression has lasted for a long time, psychotherapy can help break entrenched patterns of thought and behaviour. Many clients with chronic depression report noticeable improvement when therapy is consistent and tailored to their needs.
What if my depression feels too overwhelming to start therapy?
It is common for depression to make beginning therapy feel impossible. Part of therapy is addressing that very obstacle, taking one small step at a time. Even booking an initial consultation can be the start of change.
What if I don’t connect with my therapist?
A strong therapeutic relationship is one of the most important predictors of success. If you don’t feel a good fit, it’s appropriate to discuss it or seek a different therapist. The right match can make therapy much more effective.
Do I need medication or is therapy enough?
For some, psychotherapy alone is effective. Others may benefit from a combination of therapy and medication prescribed by a physician. Therapists collaborate with medical professionals when needed to ensure you receive the most appropriate care.
Is therapy confidential?
Yes. Sessions are private and protected by law, with very limited exceptions for safety. Confidentiality allows you to speak openly and honestly about your struggles.
Can psychotherapy help with seasonal depression?
Yes. Seasonal Affective Disorder (SAD) is a type of depression that appears during certain times of the year, most often in the fall and winter when daylight is reduced. Symptoms include low mood, fatigue, oversleeping, and changes in appetite. Psychotherapy can help by addressing negative thought patterns, building coping strategies, and supporting lifestyle adjustments. It can also be combined with treatments like light therapy and medical care for a more complete approach.
How We Approach Depression Treatment
Depression can feel overwhelming, affecting energy, motivation, and relationships, but effective care is available. Psychotherapy helps uncover the thought patterns that keep depression in place, such as hopelessness, self-blame, and avoidance, while teaching practical skills to challenge and reframe them. Many approaches also include mindfulness and acceptance strategies that make difficult emotions more manageable.
Alongside therapy, everyday habits can play a powerful role in recovery. Engaging in purposeful activities, maintaining steady sleep and nutrition, staying physically active, and building supportive connections all contribute to lifting mood and restoring balance. At our Toronto clinic, we provide evidence-based therapy for depression to help you regain stability and improve quality of life.
Seeking for Depression Treatment in Toronto?
Addy Psychotherapy is committed to delivering compassionate, evidence-based care for adults experiencing depression. We provide depression therapy in Toronto for individuals aged 18–65 who are navigating the challenges and impact of depressive symptoms. Our therapeutic approach draws on proven methods such as Cognitive Behavioural Therapy (CBT), Acceptance and Commitment Therapy (ACT), Dialectical Behaviour Therapy (DBT), and other evidence-based practices to create a treatment plan tailored to your needs. Our experienced therapists offer depression therapy in Toronto both in-person and online, making support accessible to clients across Ontario.